Continued Stress in the Exhaustion Stage Leads to
Hormones and Stress
-
2.7 Describe how the autonomic nervous system and body are impacted by stress.
The sympathetic and parasympathetic systems, and various hormones, figure prominently in our body's physiological reactions to stress.
The General Adaptation Syndrome
Endocrinologist Hans Selye was the founder of the field of research concerning stress and its effects on the human body. He studied the sequence of physiological reactions that the body goes through when adapting to a stressor. This sequence (see Figure 2.10) is called the general adaptation syndrome (GAS) and consists of three stages (Selye, 1956).
Figure 2.10
General Adaptation Syndrome
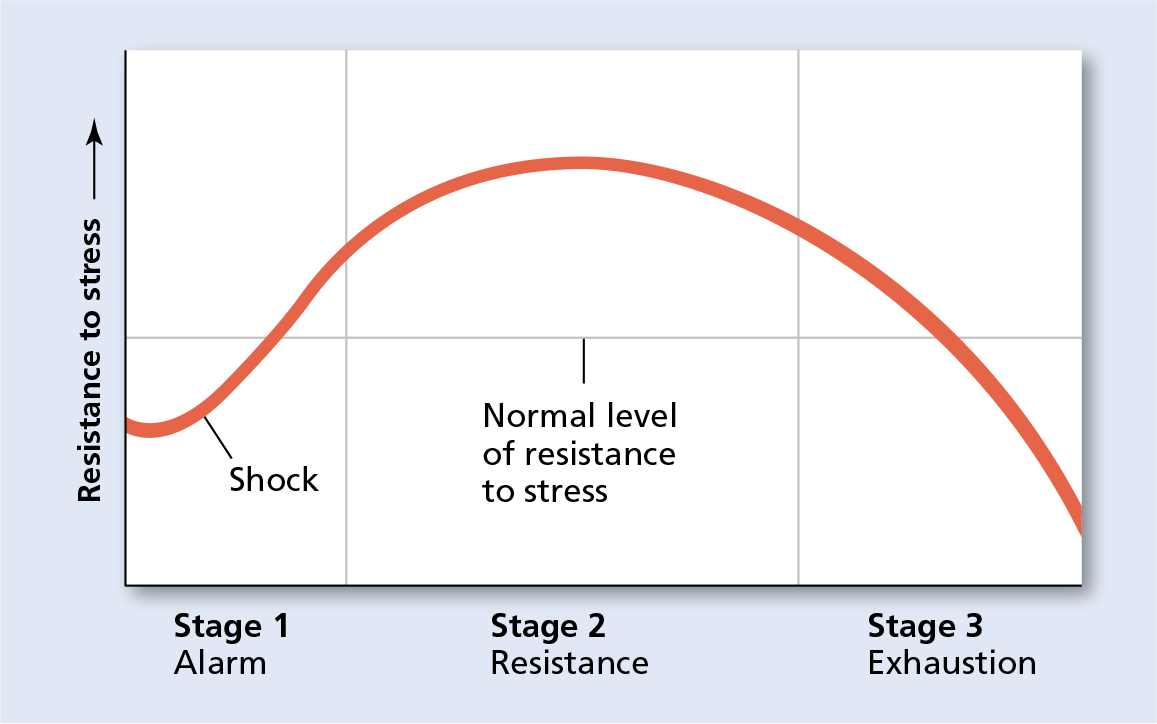
In the alarm stage, resistance drops at first as the sympathetic system quickly activates. But resistance then rapidly increases as the body mobilizes its defense systems. In the resistance stage, the body is working at a much increased level of resistance, using resources until the stress ends or the resources run out. In the exhaustion stage, the body is no longer able to resist as resources have been depleted, and at this point disease and even death are possible.
-
Alarm: When the body first reacts to a stressor, the sympathetic nervous system is activated. The adrenal glands release hormones that increase heart rate, blood pressure, and the supply of blood sugar, resulting in a burst of energy. Reactions such as fever, nausea, and headache are common.
-
Resistance: As the stress continues, the body settles into sympathetic division activity, continuing to release the stress hormones that help the body fight off, or resist, the stressor. The early symptoms of alarm lessen and the person or animal may actually feel better. This stage will continue until the stressor ends or the organism has used up all of its resources. Researchers have found that one of the hormones released under stress, noradrenaline (norepinephrine), actually seems to affect the brain's processing of pain, so that when under stress a person may experience a kind of analgesia (insensitivity to pain) if, for example, the person hits an arm or a shin (Delaney et al., 2007).
-
Exhaustion: When the body's resources are gone, exhaustion occurs. Exhaustion can lead to the formation of stress-related diseases (e.g., high blood pressure or a weakened immune system) or the death of the organism if outside help is unavailable (Stein-Behrens et al., 1994). When the stressor ends, the parasympathetic division activates and the body attempts to replenish its resources.
Alarm and resistance are stages that people experience many times throughout life, allowing people to adapt to life's demands (Selye, 1976). It is the prolonged secretion of the stress hormones during the exhaustion stage that can lead to the most harmful effects of stress. It was this aspect of Selye's work that convinced other researchers of the connection between stress and certain diseases of adaptation as Selye termed them, such as high blood pressure.
Immune System and Stress
As Selye first discovered, the immune system (the system of cells, organs, and chemicals in the body that responds to attacks on the body from diseases and injuries) is affected by stress. The field of psychoneuroimmunology concerns the study of the effects of psychological factors such as stress, emotions, thinking, learning, and behavior on the immune system (Ader, 2003; Cohen & Herbert, 1996; Kiecolt-Glaser, 2009; Kiecolt-Glaser et al., 1995, 1996, 2002). Researchers in this field have found that stress triggers the same response in the immune system that infection triggers (Maier & Watkins, 1998). Certain enzymes and other chemicals (including antibodies) are created by immune cells when the immune cells, or white blood cells, encounter an infection in the body. The white blood cells surround the bacteria or other infectious material and release the chemicals and enzymes into the bloodstream. From there, these chemicals activate receptor sites on the vagus nerve, the longest nerve that connects the body to the brain. It is the activation of these receptor sites that signals the brain that the body is sick, causing the brain to respond by further activation of the immune system.
Stress activates this same system but starts in the brain rather than in the bloodstream. The same chemical changes that occur in the brain when it has been alerted by the vagus nerve to infection in the body occurred in laboratory animals when they were kept isolated from other animals or given electric shocks (Maier & Watkins, 1998). This has the effect of "priming" the immune system, allowing it to more successfully resist the effects of the stress, as in Selye's resistance stage of the GAS.
Hormones also play a part in helping the immune system fight the effects of stress. Researchers (Morgan et al., 2009) have found that a hormone called dehydroepiandrosterone (DHEA), known to provide antistress benefits in animals, also aids humans in stress toleration—perhaps by regulating the effects of stress on the hippocampus (part of the limbic system). (See Learning Objective 2.11.)
The positive effects of stress on the immune system only seem to work when the stress is not a continual, chronic condition. As stress continues, the body's resources begin to fail in the exhaustion phase of the general adaptation to stress (Kiecolt-Glaser et al., 1987, 1995, 1996; Prigerson et al., 1997). In one study, college students who were undergoing a stressful series of exams were compared to a group of similar students relaxing during a time of no classes and no exams (Deinzer et al., 2000). The exam group tested significantly lower for immune system chemicals that help fight off disease than did the relaxing control group, even as long as 14 days after the exams were over. The suppression of immune system functioning by stress apparently can continue even after the stress itself is over.
One reason that the early stress reaction is helpful but prolonged stress is not might be that the stress reaction, in evolutionary terms, is really only "designed" for a short-term response, such as running from a predator (Sapolsky, 2004). That level of intense bodily and hormonal activity isn't really meant to go on and on, as it does for human beings in the modern, stress-filled life we now know. Humans experience the stress reaction over prolonged periods of times and in situations that are not necessarily life-threatening, leading to a breakdown in the immune system.
Heart Disease
Of course, anything that can weaken the immune system can have a negative effect on other bodily systems. Stress has been shown to put people at a higher risk of coronary heart disease (CHD), the buildup of a waxy substance called plaque in the arteries of the heart. This relationship is at least in part because the liver, which is not activated while the sympathetic nervous system is aroused, does not have a chance to clear the fat and cholesterol from the bloodstream, leading to clogged arteries and eventually the possibility of heart attacks or strokes. In one study, middle-aged men were questioned about stress, diet, and lifestyle factors and were examined for biological risk factors for heart disease: obesity, high blood sugar, high triglycerides (a type of fatty acid found in the blood), and low levels of HDL or "good" cholesterol. (See Figure 2.11) Stress and the production of stress hormones were found to be strongly linked to all four biological risk factors: The more stress the men were exposed to in their work environment and home life, the more likely they were to exhibit these risk factors (Brunner et al., 2002).
Figure 2.11
Stress and CHD
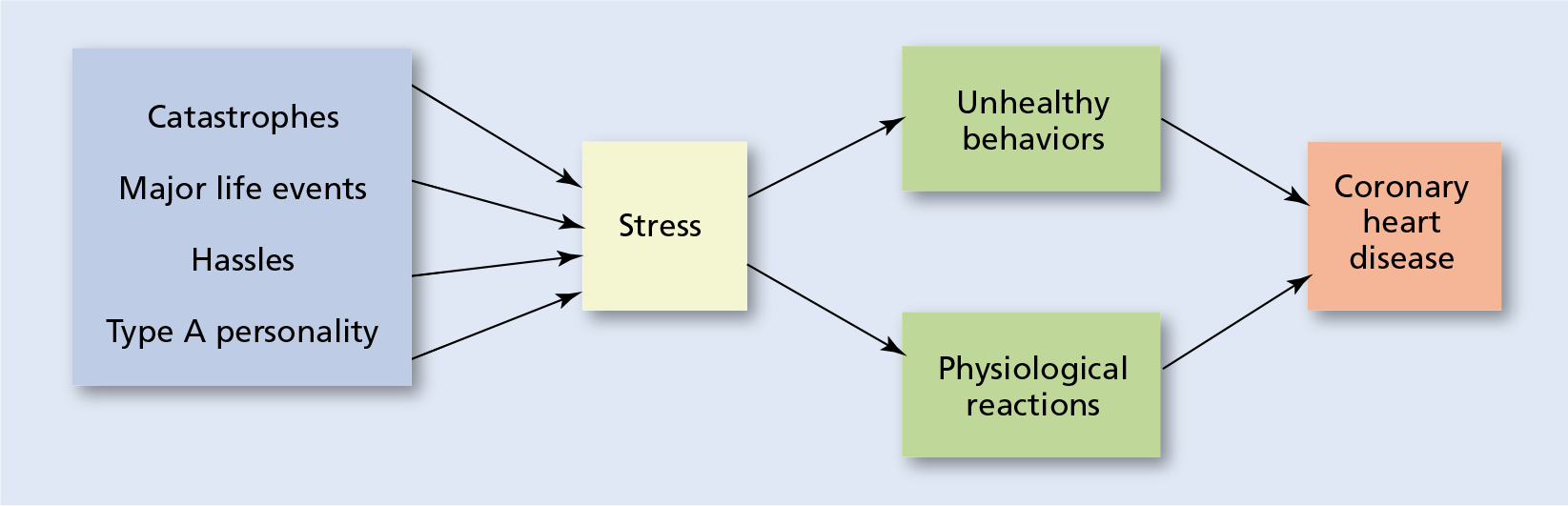
The blue box on the left represents various sources of stress (Type A personality refers to someone who is ambitious, always working, and usually hostile). In addition to the physical reactions that accompany the stress reaction, an individual under stress may be more likely to engage in unhealthy behavior such as overeating, drinking alcohol or taking other kinds of drugs, avoiding exercise, and acting out in anger or frustration. This kind of behavior also contributes to an increased risk of coronary heart disease.
Other studies have produced similar findings. One study looked at the heart health of people who suffered acute stress reactions after the 9/11 terrorist attacks and found a 53 percent increase in heart ailments over the 3 years following the attacks (Holman et al., 2008), whereas another large-scale study found that work stress is highly associated with an increased risk of coronary heart disease due to negative effects of stress on the autonomic nervous system and glandular activity (Chandola et al., 2008). Recent studies have shown a clear relationship between stress in the workplace and an increased risk of coronary heart disease as well as depression, sleep disturbances, and unhealthy habits such as a lack of physical activity—none of which are good for coronary health (Emeny et al., 2012, 2013). Prolonged stress is simply not good for the heart.
Cancer
Cancer is not one disease but rather a collection of diseases that can affect any part of the body. Unlike normal cells, which divide and reproduce according to genetic instructions and stop dividing according to those same instructions, cancer cells divide without stopping. The resulting tumors affect the normal functioning of the organs and systems they invade, causing them to fail, eventually killing the organism.
Although stress itself cannot directly give a person cancer, stress can have a suppressing effect on the immune system, making the unchecked growth of cancer more likely. In particular, an immune-system cell called a natural killer (NK) cell has as its main functions the suppression of viruses and the destruction of tumor cells (Herberman & Ortaldo, 1981). Stress has been shown to depress the release of natural killer cells, making it more difficult for the body's systems to fight cancerous growths (Zorilla et al., 2001). The hormone adrenaline is released under stress and has been found to interfere with a protein that normally would suppress the growth of cancer cells (Sastry et al., 2007). In other research, stress has been linked to the release of hormones such as adrenaline and noradrenaline that, over time, can cause mistakes (such as damage to the telomeres, structures at the ends of chromosomes that control the number of times a cell can reproduce) in the instructions given by the genes to the cells of the body. As these mistakes "pile up" over the years, cells can begin to grow out of control, causing the growth of tumors and possibly cancer (Kiecolt-Glaser et al., 2002).
Stress may impact the effectiveness of cancer treatments as well. In one study of mice implanted with human prostate cancer cells, treatment with a drug to destroy the cancer cells and prevent growth of tumors was effective when the mice were kept calm and stress-free, but failed miserably when the mice were stressed (Hassan et al., 2013).
One possible bit of positive news: Unlike the research linking stress at work to heart disease and diabetes, one study has found that work-related stress does not appear to be linked to developing cancer of the colon, lungs, breasts, or prostate (Heikkila et al., 2013). While 5 percent of over 100,000 participants in the 12 years over which the study took place developed some form of cancer, there was no association between job-related stress and risk of cancer.
Other Health Issues
Heart disease and cancer are not the only diseases affected by stress. As indicated earlier, weight problems may also become associated with stress. One chronic illness sometimes associated with excessive weight gain is diabetes, specifically Type 2 diabetes (Type 1 diabetes is associated with failure of the pancreas to secrete enough insulin, necessitating medication, and is usually diagnosed before the age of 40). Type 2 diabetes is associated with excessive weight gain and occurs when pancreas insulin levels become less efficient as the body size increases. Type 2 diabetes can respond favorably to proper diet, exercise, and weight loss, but may also require medication. Typically, it is associated with older adults, but with the rise in obesity among children, more cases of Type 2 diabetes in children are now occurring.
Research has continued to link high levels of stress with increased risk of diabetes. A 35-year study in Sweden monitored the health and stress factors of 7,500 men who began the study with no history of diabetes or coronary heart disease (Novak et al., 2013). Those men who reported experiencing permanent stress, related to home life and/or work life, had a 45 percent higher chance of developing diabetes compared to men who reported no stress or only periodic stress. Another study found that high levels of stress in the workplace can accurately predict who will develop diabetes, particularly in those people who had low levels of social support (Toker et al., 2012).
Studies have shown that children in families experiencing ongoing stress are more likely to develop fevers with illness than are other children (Wyman et al., 2007). (Oddly enough, this same study showed that in children, stress actually seems to improve the function of their natural killer cells, just the opposite effect that is seen in adults.) A review of research and scientific literature (Cohen et al., 2007) found stress to be a contributing factor in a variety of human diseases and disorders, including heart disease, depression, and HIV/AIDS. Another longitudinal study's findings suggest that experiencing work-related stress in middle age may increase an individual's chances of developing both physical and mental disabilities in old age (Kulmala et al., 2013).
Concept Map 2.6
Click or Tap the Start Button to Explore the Concept and + to Expand.
Concept Map 2.7
Click or Tap the Start Button to Explore the Concept and + to Expand.
Source: https://revelpreview.pearson.com/epubs/pearson_ciccarelli_pae/OPS/xhtml/ch02_sec_10.xhtml
0 Response to "Continued Stress in the Exhaustion Stage Leads to"
Post a Comment